Multimodal physical activities, those that include balance, aerobic, and muscle strengthening components (United States Department of Health and Human Services, 2018), can attenuate the physiological declines associated with aging (Chodzko-Zajko et al., 2009; Howe et al., 2011) and are recommended to preserve function and reduce fall risk (Chodzko-Zajko et al., 2009; Gillespie et al., 2012; United States Department of Health and Human Services, 2018). Golf is a lifespan multimodal physical activity that includes walking, bending, putting, and swinging. Walking during a single round of golf meets the American College of Sports Medicine guidelines for weekly cardiovascular physical activity in older adults (Broman et al., 2004). Bending over to tee up, mark, or retrieve the golf ball requires both balance and lower-extremity strength. The putt requires static postural control (Hurrion, 2009), while the golf swing is a high velocity movement (Lynn et al., 2013) that requires dynamic postural control in the form of a bilateral weight shift (Ball & Best, 2007). The hips generate the power for the golf swing resulting in large hip kinetic demands in the sagittal and frontal planes (Foxworth et al., 2013).
Older military Veterans, as compared to non-Veterans, have poorer health and fewer are meeting the weekly physical activity recommendations (Hoerster et al., 2012; Littman et al., 2009). Commencement of a regular multimodal activity program may help to attenuate the physiological declines in older military Veterans, translating to improved health and function across the lifespan. Cross-sectional data reveals that older golfers have better balance during static and dynamic tasks than healthy, older controls and similar balance to older adults that regularly practice Tai Chi (Gao et al., 2011; Tsang & Hui-Chan, 2004, 2010). In Japan, older adults whom regularly golf report greater self-reported health, less depressive symptoms, and more laughter than non-golfing counterparts (Tsuji et al., 2020). In the United Kingdom, golfers self-report greater personal well-being than the general population (Sorbie et al., 2020). Golf has been utilized as a cognitively-focused activity intervention for older adults (Shimada et al., 2018), though it remains to be seen whether it can also be used to improve balance, strength, and physical function in older adults (Murray et al., 2017). Therefore, the overall objective of this study was to investigate the effects of a comprehensive golf training program on measures of physical performance, including hip-abductor performance and dynamic balance, in current non-golfing, older military Veterans. It was hypothesized that measures of physical performance and dynamic balance would improve following the golf training program. Additionally, it was hypothesized that hip abductor muscle performance would also improve and contribute to the hypothesized improvements in physical performance and dynamic balance.
Methods
Experimental design
A Phase I, within-subjects, longitudinal study was used to compare measures of physical performance, dynamic balance, and hip abductor muscle performance before and after a twelve-week comprehensive golf training program (Du Bois et al., 2019). All testing occurred within two weeks of commencement and completion of the program.
Participants
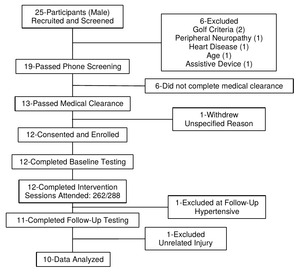
Twenty-five healthy, older (60-80 years) military Veterans that could ambulate independently and were not currently golfing were recruited to participate in the Golf Intervention for Veterans Exercise (GIVE) Study (Figure 1) (Du Bois et al., 2019). They were excluded if they had any injuries/medical conditions that could make it unsafe to participate (Du Bois et al., 2019). Following a two-part screening process, twelve male military Veterans (Age: 70.8 ± 4.9 y; Height: 1.77 ± 0.06 m; Mass: 101.0 ± 25.9 kg) were enrolled in the study. Eight of the twelve participants had no golf experience in the previous twenty years. Of the four with golf experience, one participant visited a driving range in the previous year and one participant visited a driving range and played golf in the previous 5 years. The remaining two participants visited a driving range and played golf in the previous 20 years.
All eligible participants were informed of the details of the study as approved by the Institutional Review Board (IRB) at the University of Southern California Health Sciences Campus and the IRB and Associate Chief of Staff for Research and Development at the Veterans Affairs West Los Angeles Medical Center (WLAVA), and provided their consent to participate.
Comprehensive Golf Training Program
Participants completed a twelve-week comprehensive training program that met twice weekly for 90 minutes per session. All training took place at the Heroes Golf Course, a nine-hole, Par 3 golf course located at the WLAVA. The comprehensive golf training program consisted of complementary exercises that prepared participants for the demands of golf, a dynamic warm-up, golf skill training, and progressive golf play. As the study progressed, complementary exercise time decreased while golf play increased, allowing participants to play a full round of golf (9 holes) by the final session. Full details of the comprehensive golf training program have been previously published (Du Bois et al., 2019).
Adherence. To assess the feasibility of the program, the number of sessions each participant attended was recorded. Additionally, to assess the safety of the program, all adverse events related to the program were also recorded.
Procedures
Before and after the comprehensive golf training program, participants underwent physical performance and dynamic balance testing on separate days. Before physical testing was performed, blood pressure and heart rate were measured to verify inclusion/exclusion criteria. Participants began testing with a warm-up that consisted of 30-seconds of marching in place, 5 chair stands, and another 30-seconds of marching in place.
Physical Performance. Physical performance measures included the 30-second chair stand and 8-foot-up-and-go test, which are components of the Senior Fitness Test (Rikli & Jones, 2013). Participants performed one trial of the 30-second chair stand and two trials of the 8-foot-up-and-go test after a brief familiarization with the tests (Rikli & Jones, 2013).
Dynamic Balance. Dynamic balance was assessed via a rapid step test. Participants began standing with their feet shoulder width apart and each foot on a separate AMTI embedded force platform (1500 Hz; OR-6-1000; Newton, MA). Participants received a red warning light followed by either a yellow or green light (within 3 seconds), indicating that the participants were to step as quickly as possible, with either their left limb or right limb, respectively, onto an elevated force platform (15 cm high) placed 15 cm anteriorly (Figure 2) (Brauer et al., 2000). Participants were instructed to start with equal weight on each limb and to place their entire foot onto the step. Five practice trials were performed followed by 10 trials per limb (20 total) in a randomized order. Foot position was recorded and marked to ensure a similar starting position across trials and pre-post visits.
Hip Abductor Muscle Performance. Using previously published methodology, participants stood with their feet shoulder width apart, knees vertically aligned over their toes (pointed straight ahead) while standing in a semi-squat position (50° of knee flexion and 30° of hip flexion, confirmed by goniometry), and arms folded across the chest (Lee & Powers, 2013). The weight-bearing testing position was similar to a golf stance and thus tested the hip abductors in a functional position. An uniaxial force transducer (model LCCA-1K; OMEGA Engineering, Inc, Stamford, CT) connected to an inelastic fabric strap was secured around the thighs just above the femoral epicondyles. Strap length, transducer location, and foot width were recorded to ensure similar strap placement during the post-training testing.
Following three submaximal practice trials (approximately 50%, 75% and 90% of perceived maximal effort), participants began the testing trials with a minimal amount (average 9 ± 3 N) of baseline tension to remove slack in the strap. Participants were instructed to “push as quickly and as forcefully as possible” and to maintain this maximum effort for 5 seconds. Visual feedback of the force tracing was provided with Qualisys Track Manager Software (Qualisys AB, Gotëborg, SE) and it was explained that the goal was to get the line as steep and as high as possible. Verbal encouragement was also provided to ensure maximal effort. A total of six trials were collected.
Data analysis
Physical Performance. The total number of completed chair stands was recorded for analysis during the 30-second chair stand. The best performance of the two test trials for the 8-foot-up-and-go test was used for analysis.
Dynamic Balance. Ground reaction force (GRF) data were filtered with a fourth-order zero lag Butterworth filter with a cut-off frequency of 50 Hz. All trials were visually inspected and trials where participants reacted/stepped in response to the warning light were discarded. The step test was divided into a weight shift phase and a step phase. The onset of the weight shift was defined as the point where the vertical GRF under the swing (stepping) limb diverged three standard deviations from baseline (baseline = average GRF during the 500 ms period prior to the cue signal) for more than 50 ms (MacKinnon et al., 2007). The end of the weight shift and the start of the step was defined by toe off of the swing limb (GRF < 20 N), whereas the end of the step was defined as foot contact with the step (GRF > 20 N). Temporal measures included weight shift time (weight shift start to end), step time (step start to end), and movement time (start of weight shift to end of step) (Figure 2). The five fastest movement time trials for the dominant limb, defined as the preferred kicking limb, were used for analysis. All participants were right limb dominant.
Hip Abductor Muscle Performance. Data was sampled at 1500 Hz on a 16-bit external analog-to-digital board, converted to Newtons via a calibration factor, and normalized to body mass. All trials were visually inspected and trials with a countermovement (e.g. rapid decrease in force before contraction) were discarded (Aagaard et al., 2002). Peak force was calculated as the highest force output over the 5-second contraction. The average rate of force development was calculated as the average slope of the force-time curve during the first 200 ms of the force production (Aagaard et al., 2002) and force production onset was defined by a threshold equivalent to three standard deviations above the baseline force (Maffiuletti et al., 2016). The trial with the highest peak force was used for analysis (Häkkinen et al., 1998).
Statistical Analysis
Means and standard deviations (SD) were calculated for each of the dependent variables, and each was assessed for normality via visual inspection of histograms, analysis of skewness and kurtosis, and the Shapiro-Wilk test of normality. Paired-samples t-tests were used to assess the differences between baseline (Pre) and follow-up (Post) testing for variables that were normally distributed; these included hip abductor muscle performance outcomes, all step test measures, and chair stand repetitions. The 8-foot-up-and-go test time was not normally distributed; thus, a related-samples Wilcoxon signed ranks test was used. The a priori alpha (α) was set at 0.05. Cohen’s d effect sizes (d) were calculated to assess the strength of the differences. An effect size of 0.2 was considered ‘small’, 0.4 ‘medium’, and 0.8 ‘large’ (Cohen, 1988). Statistical analyses were performed using PASW software (version 18, IBM Corp., Chicago, IL) and G*Power 3 (Brunsbüttel, DE) (Faul et al., 2007).
Results
The 12 enrolled participants attended 262 of the 288 sessions for an average attendance of 91.0 ± 8.1% (range: 75% - 100%) with 8 participants attending at least 90% of the sessions. There were no program-related adverse events and no participants withdrew from the study. On the day of follow-up testing, one participant was excluded because his blood pressure was outside of the inclusion range. Additionally, one participant sustained a recent knee injury, unrelated to participation in the study, and could not safely and adequately perform the follow-up tests. Finally, one participant with existing knee osteoarthritis, reported pain while attempting the chair stand, 8-foot-up-and-go, and hip abductor tests; however, he was able to complete rapid step test without discomfort. Thus, data from a total of 10 participants are reported for the step test; whereas data from a total of 9 participants are reported for all other tests.
Physical Performance
Physical performance scores are presented in Figure 3. The number of repetitions performed during the 30-second chair stand increased by 15.9% (t(8) = -3.162, p = .013, d = 1.05) with a large effect size. 8-foot-up-and-go time improved by 13.3% (z(8) = -2.668, p =.008, d = 1.62) with a large effect size.
Dynamic Balance
Step test results are presented in Table 1. Step time improved by 8.9% with a large effect size following the golf training program (t(9) = 3.619, p = .006, d = 1.14). Movement time improved by 6.8% (t(9) = 3.057, p = .014, d = .97) with a large effect size.
Weight shift time did not significantly improve following the golf training program, despite the medium effect size (t(9) = 2.140, p = .061, d = .68).
Hip Abductor Muscle Performance
Hip abductor peak force (Pre: 2.46 ± 0.57 N/kg, Post: 2.52 ± 0.73 N/kg; t(8) = -.691, p = .509, d = .23) and average hip abductor rate of force development (Pre: 7.25 ± 2.04 N/s/kg, Post: 7.39 ± 1.69 N/s/kg; t(8) = -.281; p = .786, d =.09) did not change.
Discussion
Older military Veterans who were not current golfers were able to complete the comprehensive golf-training program with high adherence and without any program-related adverse events. Moreover, following 12-weeks of instruction and training, the participants improved their physical performance and dynamic balance.
The participants in the study attended an average 91% of the sessions and all participants attended at least 75% of sessions. A systematic review reported an average adherence to community-based group exercise interventions in older adults of 69.1% ± 14.6% with a range of 53% - 93% (Farrance et al., 2016). High adherence (93%) in previous activity studies was attributed to the reported enjoyment in the program resulting from fun and social support (Fox et al., 2007). Investigations as to why older people golf emphasize the feelings of vigor and youthfulness that result from the competitive aspects of the sport (Berlin & Klenosky, 2014) and the importance of playing with others, which facilitated relationships, provided support, and made it fun (Stenner et al., 2016). Additionally, older golfers report higher frequency of laughter and less depressive symptoms than older non-golfers (Tsuji et al., 2020). Thus, it is hypothesized that the social and competitive aspects of the comprehensive golf training program created an environment that boosted adherence in our participants.
The significant improvements in measures of physical performance in study participants may be associated with enhanced function. In previous reports, lower-extremity power training in older adults significantly increased chair stand performance 22% - 42.9% and reduced 8-foot-up-and-go time 10 – 15.3%, while traditional strength training had no effect on these measures (Bottaro et al., 2007; Lopes et al., 2016). Additionally, chair stand performance improved (27%) and 8-foot-up-and-go time was reduced (11 and 22%) following 8 months and 10 weeks of multimodal exercise training in sedentary older adults, respectively (Carvalho et al., 2009; Toto et al., 2012). The participants in the present study demonstrated similar improvements in chair stand performance (16%) and 8-foot-up-and-go time (13%), as reported for the power training and multimodal exercise groups. Furthermore, while it is uncertain how the changes in chair stand performance directly relate to function and quality of life in these military Veterans, increases greater than or equal to 2 repetitions are associated with improvements in self-reported function in patients with hip osteoarthritis (Wright et al., 2011). Six of the nine participants achieved the clinically important improvement in their repeated chair stand ability. While unaware of published clinically important improvements for the 8-foot-up-and-go test, eight of the nine participants achieved a time during the follow-up testing that was quicker than the time associated with a risk for functional mobility impairments (Rikli & Jones, 2013).
Step initiation, a functional activity reliant upon dynamic balance, requires a bilateral weight shift in the frontal plane, similar to the weight shift of the golf swing (Patla et al., 1993). This is coordinated with activation of the hip abductors and adductors (Brauer et al., 2000). The rapid step can be analyzed in two phases, the weight shift phase and the step phase. During a rapid forward step, older adults, as compared to young adults, have a slowed weight shift time and time to peak force, indicative of impaired weight shift dynamics (Patla et al., 1993). Following 12-weeks of multimodal exercise training composed of resistance, agility, and coordination exercise with an emphasis on the ankle plantarflexors, there was a 16% decrease in weight shift time during a rapid step forward test; however, there were no differences in improvement between the control group and the intervention group (Bohrer et al., 2019). A decrease in weight shift time following the intervention was anticipated given the similarity between the weight shift demands of the golf swing (Ball & Best, 2007) and a rapid step (Patla et al., 1993). Contrary to our hypothesis, the time to execute the weight shift did not significantly change following the intervention. However, the performance of our participants at baseline was similar to previously published weight shift times in healthy, young adults (Sims & Brauer, 2000) potentially creating a “ceiling effect.”
While there were no changes in the weight shift following the program, participants performed the step portion of the test faster. Additionally, the trend towards improved weight shift time and the significant decrease in step time resulted in statistically significant decrease in total movement time. Following 12-weeks of multimodal training with an emphasis on the ankle plantarflexors, older adults decreased their step time by 19% during a rapid forward step (Bohrer et al., 2019). Similarly, the participants in this study decreased their step time by 9% during a rapid step up test, which has been shown to be a more postural challenging task as compared to a rapid forward step (Sims & Brauer, 2000). Following completion of the program, the older military Veterans in this study were able to execute the step phase as quickly as previously published data in healthy, young adults (0.303 ± 0.065 s versus 0.298 ± 0.52 s, respectively) (Sims & Brauer, 2000) and older non-falling females (0.317 ± 0.015 s) (Brauer et al., 2000).
Postural control is multifaceted and relies upon vestibular, somatosensory, and visual sensory systems (Manchester et al., 1989). Cross-sectional studies demonstrate that experienced older golfers perform better on a Sensory Organization Test in the presence of conflicting somatosensory and/or visual information and demonstrate better knee joint proprioception compared to healthy, older adults (Gao et al., 2011; Tsang & Hui-Chan, 2004). The authors suggested that: “Walking over uneven ground and repeated golf swings might thus be expected to improve balance control through constant stimulation of the visual and vestibular systems” (Gao et al., 2011). Thus, the demands of golfing including walking, the golf swing, and the repeated practice of bending over to tee-up, pick up, and mark the golf ball’s placement on the greens, likely contributed to the observed changes in dynamic balance as demonstrated by the 8-foot-up-and-go test and the rapid step test.
Alongside the improvements in measures of physical performance and dynamic balance, increased peak hip abductor force and rate of force development were anticipated following the golf training program. These hypotheses were based on the knowledge that the golf swing is a high velocity movement (Lynn et al., 2013) initiated by the hip musculature (Bechler et al., 1995) and previous evidence of improved muscle performance in older adults following low load, high velocity resistance training programs (Kobayashi et al., 2016). Additionally, the hip abductors are biomechanically and functionally related to dynamic balance in the frontal plane during functional activities such as gait and gait initiation (Rogers & Pai, 1993; Sims & Brauer, 2000; Winter, 1995); thus, it was hypothesized that the changes in dynamic balance could be related to improvements in hip abductor muscle performance. Contrary to the hypotheses, there were no significant changes in hip abductor performance. Although previous studies in experienced older golfers confirmed that the hips generate the power for the golf swing and therefore have high frontal plane kinetic demands (Foxworth et al., 2013), it is possible these demands may be reduced in novice golfers learning how to play. Following eight weeks (3 days/week) of a low dose (15 minutes/session) hip abductor power training (standing hip abduction on a pneumatic cable resistance machine) in older adults, peak isometric hip abductor torque improved 14% and hip abductor rate of torque development increased 39% (Inacio et al., 2018). Additionally, knee osteoarthritis patients (50 years and older) completing 12 weeks (5 days per week) of hip abductor strengthening (side lying and standing exercises with ankle weights and resistance bands) significantly improved their peak isometric hip abductor force 13% (Bennell et al., 2010). The reduced frequency (2 days versus 3 to 5 days per week), differing type of exercise stimulus, and the potential reduction in exercise intensity in this study could have contributed to the lack of observed changes in hip abductor muscle performance as compared to those reported in hip abductor-specific strength training studies.
The hip abductor assessment was chosen because it is a validated assessment of hip abductor muscle performance and is performed in a functional, weight-bearing position similar to the golf stance (Lee & Powers, 2013). Nevertheless, the isometric nature of the test may have limited the ability to detect changes in hip abductor muscle performance because of the dynamic nature of the golf training program. Given the importance of muscle power preservation for older adult functional capabilities (Bean et al., 2002), the inclusion of assessments of hip abductor power (e.g. isokinetic tests at various contraction velocities) are warranted and likely to provide additional information regarding the effects of multimodal training programs on lower-extremity muscle performance.
One limitation of this study is the small sample size; however, it is not believed that this study was underpowered. A-priori power analyses based on pilot data from two participants revealed that a minimum four people would be required reach a significance level of 0.05 with an estimated power of 80%. Additionally, a post-hoc power analysis revealed that more than 150 participants would be required to detect changes in hip abductor muscle performance and 20 participants would be required to detect changes in weight shift time. Thus, a large number of participants would be required to find small, yet significant differences, which may not be clinically meaningful. The use of older, male military Veterans may limit the ability to extrapolate the findings to a larger cohort of older adults that includes females. Additionally, participants in the program had varying physical activity habits raging from sedentary to active. Participants did not begin any new exercise or activity routines over the course of the training program, but prior activity levels could have affected the response to the program. Future research should investigate the effectiveness of comprehensive golf training programs on balance and strength in larger cohorts of older military Veterans including females while also expanding to community-dwelling older adults.
It cannot be definitively stated which aspects of the golf training program were responsible for the observed changes in physical performance and dynamic balance. The multiple demands of the golf training program included walking over hilly, uneven, and varying terrain, bending over to pick up or place a golf ball, static putts, and ballistic golf swings. The complementary exercise training and dynamic warm-up likely also played a role in the observed changes. The findings of this study are supported by meta-analyses and systematic reviews of multimodal exercise programs, which support high adherence rates and demonstrate improvements in balance, physical performance, and reduced fall risk (Bouaziz et al., 2016; Chodzko-Zajko et al., 2009; Farrance et al., 2016; Gillespie et al., 2012; Howe et al., 2011). Finally, although the study did not include a control group, this Phase I pre-post study design was used to investigate the feasibility and safety of a novel golf intervention program for older military Veterans, and to determine the strength and balance effect sizes in accordance with National Institutes of Health (NIH) recommendations for the development of larger clinical trials (National Institutes of Health, 2017).
Conclusion
The results from our study demonstrate that a comprehensive golf training program is a feasible, safe, and effective exercise intervention for older military Veterans. The program specifically increased the number of repetitions performed during a 30 second chair stand, which is indicative of improved strength and power. Participants also significantly reduced step and movement time during a rapid step test and time to complete an 8-foot-up-and-go, indicative of enhanced dynamic balance and agility. Overall, the observed improvements have important implications for preserving function and reducing fall risk in older military Veterans.
Acknowledgements
The authors thank the military Veterans that graciously volunteered their time to the GIVE Study, Erin Blanchard for help with the therapeutic exercises, and James Dennerline for leading the golf training.


_and_8-foot-up-and-go_time_(b)_before_(pre)_and_after_(post.png)

_and_8-foot-up-and-go_time_(b)_before_(pre)_and_after_(post.png)