Older adults experience physiological and cognitive changes that impair their ability to perform activities of daily living and increase their risk for falls (Tinetti et al., 1988). Among this population of older adults, military Veterans are more likely to report poorer health and limitation of activities, and are more likely to have cardiovascular disease, cancer, arthritis, and a history of anxiety/depressive symptoms compared to non-Veterans (Hoerster et al., 2012). Moreover, few military Veterans are meeting current physical activity recommendations (Littman et al., 2009). In order to attenuate the declines in health and independence, older adults should participate in regular physical activities (United States Department of Health and Human Services, 2018). Multimodal physical activities are those which simultaneously incorporate several components of a fitness program—balance, strength, gait, and agility training. These comprehensive programs improve functional fitness and balance in older adults and are recommended to reduce fall risk and fall rate (Bouaziz et al., 2016; Chodzko-Zajko et al., 2009; Gillespie et al., 2012; Zimmer et al., 2017).
Golf is a popular multimodal recreational activity that can be played across the lifespan (Stenner et al., 2016). Walking a golf course is considered moderate to vigorous aerobic exercise in older adults, and a single round of golf can meet the American College of Sports Medicine (ACSM) guidelines for weekly cardiovascular exercise (Broman et al., 2004; Stauch et al., 1999), translating to improved cardiovascular health and body composition (Palank & Hargreaves, 1990; Parkkari et al., 2000). Golf also requires the golfer to bend over numerous times to pick up or put down a ball using movement patterns (e.g., squat & lunge) similar to strengthening exercises (Du Bois & Salem, 2015). The putt requires static postural control as the golfer minimizes the movements of the center of pressure to precisely execute the shot (Hurrion, 2009), whereas the golf swing is a ballistic and muscularly demanding movement that requires the coordination of numerous segments of the body as they travel through a large range of motion at a rapid velocity (Bechler et al., 1995; Foxworth et al., 2013; Neal et al., 2007). The golf swing also requires dynamic balance as the golfer must perform a bilateral weight shift to execute the shot (Ball & Best, 2007). Golfers have enhanced static and dynamic balance, proprioception, and balance confidence as compared to age-matched controls, and similar balance performance to older adults that regularly practice Tai Chi (Gao et al., 2011; Tsang & Hui-Chan, 2004, 2010).
Golf is not only physically demanding, but also includes cognitive challenges. For example, golfers must assess ball position, terrain type, pin distance, wind direction, hazard location, putting break, and other environmental conditions when selecting an appropriate club, choosing swing magnitude, and executing a good shot. Moreover, because the golf swing is a highly skilled movement, learning how to swing a golf club may stimulate neuroplasticity associated with complex-motor skill learning (Bezzola et al., 2011, 2012).
Golf is typically played in groups of 2-4 people, and thus requires social engagement, which has been reported to help golfers make friends, develop a support system, facilitate communication, and is simply fun (Berlin & Klenosky, 2014; Stenner et al., 2016). Additionally, the competitive aspects of golf have been ascribed to enhance feelings of self-worth, a sense of achievement, and a feeling of youth/vigor (Berlin & Klenosky, 2014).
Despite evidence of the overall health and wellness benefits of golf, golf as a health and wellness intervention has rarely been studied. Golf play was used as part of a physical therapy program for a small number of individuals following stroke, and resulted in improvements in balance, coordination, strength, and quality of life (Shatil et al., 2005; Zoerink & Carter, 2015). Currently, golf is being used therapeutically to address Parkinson’s disease, dementia, and osteoarthritis, but there is little published evidence to support anecdotal reports of improved health (Murray et al., 2016). Finally, a 24-week, one day per week cognitive-focused, golf training intervention improved logical memory in healthy, older adults with no changes in word memory, general cognition, or physical performance measures including walking speed and grip strength. However, the feasibility of implementing such a program may be challenging as the study was 24 weeks, utilized a high number of assistants (4-6 per session), and included lecturing sessions and undescribed home-based golf practice every day (Shimada et al., 2018).
Given the declines in physical and cognitive health with aging, the increased risk of falls, and the unique health concerns facing older military Veterans, we designed a Phase I longitudinal intervention study (Golf Intervention for Veterans Exercise [GIVE]) to examine the feasibility, safety, and efficacy, of a 12-week comprehensive golf training program aimed at improving the physical, cognitive, and psychosocial health of older military Veterans. A secondary aim of the study was to examine the biomechanical characteristics of the golf-related movements (swings and ball placement) and the walking distances of the participants, in order to gain a more thorough understanding of physical demands of the program. This manuscript will describe the design and implementation of the golf training program and provide a brief overview of the outcomes used to evaluate program feasibility, safety, and efficacy.
Methods
Experimental Design
Current non-golfing, older military Veterans between the ages of 60 – 80 years were recruited for the study. Following screening, consent, and enrollment, participants underwent baseline testing to evaluate their physical, cognitive, and psychosocial status. Participants then partook in a twelve-week comprehensive golf training program that met twice weekly. The comprehensive golf training program consisted of: 1) complimentary exercise training and a dynamic warm-up that prepared the participants for the physical demands of golf, 2) golf skill training, 3) an introduction to rules and etiquette, and 4) progressive golf play. Within 2 weeks after completion of the intervention, participants underwent follow-up testing to assess changes in their physical, cognitive, and psychosocial status.
Given the novelty of utilizing golf as a health intervention, a Phase I clinical trial study design was developed. This study design allowed us to: 1) determine the feasibility (including program adherence) of running a golf-training intervention for non-golfing older military Veterans, 2) evaluate if older adults could be safely instructed how to golf, and 3) determine if golf had an effect on the health status of the participants. Phase I clinical trials are essential for the refinement and standardization of the intervention before progressing to larger Phase II and III studies that include a control group, as recommended by the National Institutes of Health (2017).
Ethics Review
All eligible participants were informed of the details of the study as approved by the Institutional Review Board (IRB) at the University of Southern California Health Science Campus and the IRB and Associate Chief of Staff for Research and Development at the Veterans Affairs West Los Angeles Medical Center (WLAVA).
Participants
Eligibility criteria. Older adults were included if they 1) were military Veterans between the ages of 60 and 80 years, 2) were not currently golfing, had not golfed more than one time in the past month, and had not golfed more than three times in the past 6 months, 3) could stand and walk independently without assistance, 4) were English-speaking, and 5) had a primary care physician. Participants were excluded if they had dementia or Alzheimer’s disease; symptomatic cardiovascular disease, active angina, uncontrolled hypertension, or symptomatic hypotension; unstable asthma or exacerbated chronic obstructive pulmonary disease; rheumatoid arthritis; unstable joints; orthopedic operation within the past 6 months; movement disorders such as Parkinson’s disease or other neurological disorders; stroke, hemiparesis, or paraparesis; peripheral neuropathies; severe vision or hearing problems; metastatic cancer; and vestibular, visual, musculoskeletal, orthopedic and/or neurological disorders known to impair balance.
Power analyses were performed to determine the appropriate sample size from pilot data of two individuals using G*Power 3 (Brunsbüttel, DE) (Faul et al., 2007). The power analyses were used to detect differences in the physical measures (e.g., hip abductor muscle performance, six-minute walk), dynamic balance, and gait parameters (e.g., speed and spatiotemporal measures). Across all measures, 10 participants were needed to detect pre-post differences with a significance level set at 0.05 and estimated power of 80%. In order to account for participant drop out, 12 participants were enrolled in the study.
Recruitment and screening. Participants were recruited using physician referrals, flyers, and visits to community centers, military Veteran fitness/wellness classes, military Veteran organizations, and military Veteran housing facilities in the Greater Los Angeles area. Once identified, the participants went through a two-part screening process that included a phone interview and clearance from their primary care physician. The phone screen included the Telephone Memory Impairment Screen (Lipton et al., 2003) and a series of questions pertaining to the inclusion and exclusion criteria. Participants that passed the phone screen were then required to receive clearance from their primary care physician prior to enrollment in the study. At the baseline testing session, additional details of the study were explained to the participants, and consent was obtained by an experienced researcher.
Comprehensive Golf Training Intervention
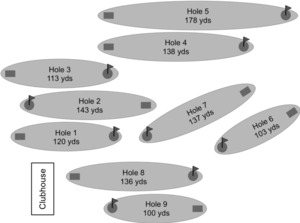
The comprehensive golf training program was designed for older adults who were not currently golfing. The program included golf-specific warm-up exercises that prepared the golfer for the flexibility, strength, and balance requirements of golf play, in conjunction with golf skill training, and a gradual introduction to golf play (Table 1). The complimentary exercises were led by a certified exercise professional, and all golf training occurred under the direct supervision of a Professional Golf Association (PGA) instructor. Groups of four participants were each provided 24 training sessions (2 sessions/week), lasting approximately 90 minutes. When the PGA instructor was unavailable due to conflicts with scheduled golf tournaments, the training was rescheduled, and the intervention continued until 24 sessions were held. Thus, the 24 sessions required 14 weeks to complete. All training occurred at the Heroes Golf Course, a Par 3, 9-hole golf course, located at the WLAVA in Los Angeles, CA (Figure 1).
In order to characterize the walking demands of the program, participants wore wrist fitness trackers (Fitbit Surge™, Fitbit, Inc., San Francisco, CA). Walking distance was calculated from the Global Positioning System (GPS) data from the Fitbits. This was done to minimize errors in distance calculations from step count out of concern that the arm movement during the golf swing could be counted as a step. Fitbit technology is the most commonly used commercial fitness activity monitor to track steps, energy expenditure, and heart rate in research protocols (Henriksen et al., 2018). Research personnel also recorded stroke count, golf score, and the number of times the participants picked up, or placed a golf ball. Stroke count included the total number of swings taken including wood and iron swings, pitch and chip shots, and putting, when contact was made with a ball. Practice swings were not included in the count.
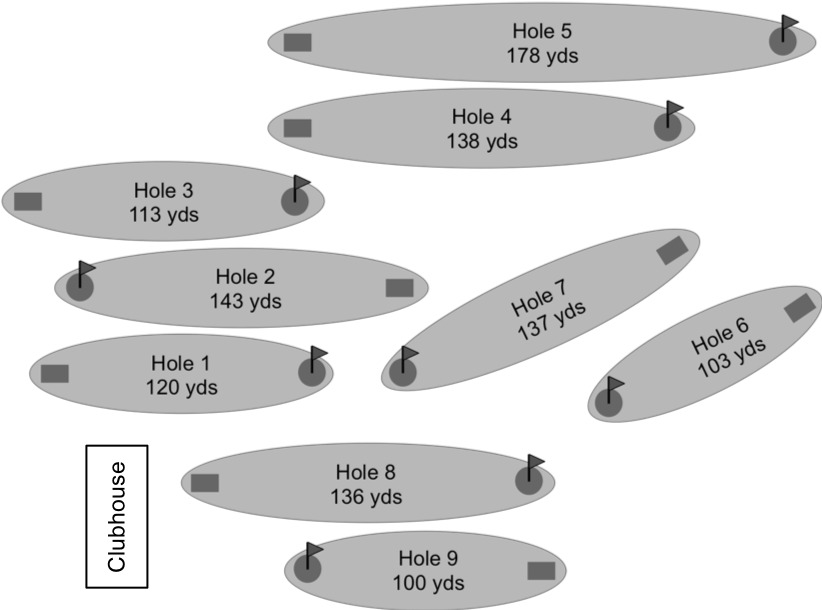
Complimentary exercise training. At the beginning of each training session, complimentary exercises and dynamic warm-up activities that mimicked the movement patterns and physical demands of golf play, were included to prepare participants for the rigors of play on the course. Exercise time was gradually reduced as the training program progressed, beginning with 45 minutes of training during the first 3 weeks and ending with a 10-minute dynamic warm-up during weeks 8-12 (Table 1).
Complimentary exercises were chosen: 1) based on electromyographical analysis of golf swing demands (Bechler et al., 1995; Pink et al., 1990), 2) previous research investigating the effects of conditioning programs on the performance and physical fitness of older golfers (Thompson & Osness, 2004), and 3) current strength and conditioning recommendations/considerations for golfers (Read & Lloyd, 2014).
Participants walked for 2-10 minutes to a private area of the golf course for the exercise and warm-up training. This pre-exercise walking time was considered an important component of the warm-up, and the duration was “regressed” from 10 to 2 minutes (411.47 ± 50.59 m to 133.71 ± 57.85 m) as the amount of actual golf play, therefore course walking time, increased over the 12-week period. Lower extremity exercises included body weight squats with heel raises and standing leg raises. Upper extremity exercises included chest fly, chest press, bent over row, and reverse fly with resistance bands. Quadruped hip extensions (with optional arm extension) and bridge were included to address hip, abdominal, and back musculature. Golf specific drills that prepared golfers for the weight shift demands of golf included a backswing loading drill, downswing loading drill, and full swing loading drill. Exercise training concluded with a latissimus dorsi/hamstring stretch and standing side stretch (Figure 2). Training consisted of 2-3 sets of 8-10 repetitions for each exercise. During the first 3 weeks, the training consisted of 2 lower body, 2 upper body, 2 abdominal/back exercises, a golf-specific drill, and stretches. During weeks 4-7, training sessions consisted of one exercise from each muscle group, one golf-specific drill, stretches, and the dynamic golf warm-up (described below).
After week 7, only a dynamic warm-up was included as part of the exercise training, which provided time for the participants to play 6-9 holes on the course. A warm-up of at least ten minutes has been shown to reduce injury risk and improve golf performance (Fradkin et al., 2004; Lindsay & Vandervoort, 2014). The dynamic warm-up included shoulder circles, triceps backswing/downswing stretch, hand/wrist-shakes, partial swings, and full swings (without ball).
Golf skill training. During the first three weeks (sessions 1-6), participants were introduced to the rules and etiquette of golf and had swing training at a modified driving range. Each day of golf skill training was spent on a specific club/swing type and participants were instructed how to putt, pitch and chip, and hit iron and wood shots. To safely introduce swings, golfers performed an average of 9.2 ± 0.7 strokes on the first day of practice and progressed to 31.1 ± 15.2 strokes on the final day of swing training. Due to the relatively low demand of chipping/pitching and putting, stroke count increased on these days (28.2 ± 8.7 strokes to 52.1 ± 20.2 strokes).
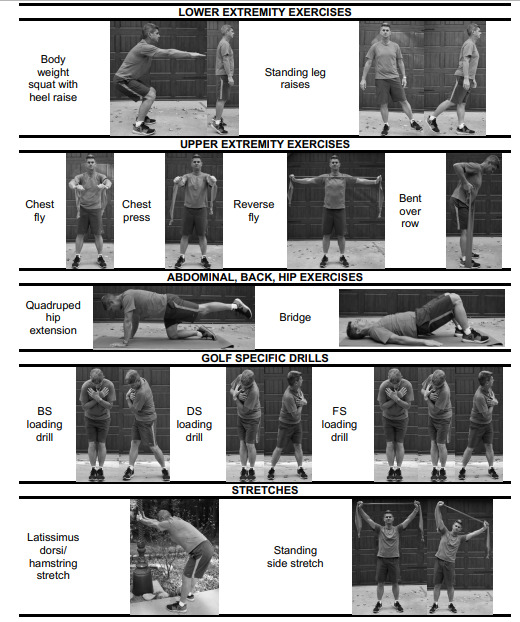
Golf play. Golfers began golf play on 2 holes in week 4 and gradually increased their amount of play to 9 holes by the final session. During all golf play, participants walked the golf course while pushing their golf clubs with a push cart. During the early weeks of the intervention, golfers played the holes closest to the clubhouse (Figure 1, holes 1-3, 8-9). As skill level and fitness progressed, golfers were introduced to holes further from the clubhouse; therefore, in general, walking distance increased as the intervention progressed (Figure 3A). This was a function of both the increasing number of holes played and play on holes further from the clubhouse. Similarly, the number of strokes taken (Figure 3B) and the number of times golfers bent over to tee-up, mark, or retrieve a golf ball (Figure 3C) also generally increased across the intervention as players played more difficult holes (e.g., holes 4 and 5, Figure 1) and a greater number of holes. During golf play, the PGA professional instructor provided information and feedback on club choice, swing mechanics, general golf etiquette, and specific golf rules as necessary. Participants were instructed not to play or practice golf outside of the golf training program.
Outcome Measures
Adherence to the intervention was tracked by recording the number of sessions attended. Adverse events were recorded to evaluate the safety of the intervention.
Performance outcomes were measured on two occasions: 1) within two weeks prior to the start of the golf training program (Pre) and 2) within two weeks of the final training session (Post). Both Pre and Post measures were performed over two days in order to minimize fatigue. Anthropometrics, physical fitness, balance, gait analysis, and golf biomechanics testing occurred at the University of Southern California Health Science Campus in Los Angeles, CA. Anthropometric measures included body mass and body composition. Physical fitness measures assessed hip abductor muscle performance and cardiovascular fitness (six-minute walk). Balance measures included balance confidence (Activities-specific Balance Confidence Scale) (Powell & Myers, 1995), semi-tandem stance and single leg stance (static balance), and a rapid step test (dynamic balance). Gait analyses assessed speed and the biomechanics of self-selected, fast, and dual-task fast gait.
Little is known about the demands of golf-related activities in novice, older golfers; therefore, the biomechanics of marking a golf ball, and the biomechanics of the golf swing with a pitching wedge, 7-iron, hybrid, and driver were also evaluated following completion of the golf training intervention. This evaluation allowed for a complete understanding of the golf-related demands and the observed physical adaptations to the golf training program.
The remaining physical performance measures, cognition, and self-reported outcomes were collected at the WLAVA on a separate day. Physical performance measures included handgrip dynamometry, 30-second chair stand (lower extremity muscle strength), and 8-foot-up-and-go (dynamic balance and agility). The California Verbal Learning Test 2nd Edition Standard Form (PsychCorp, Pearson, Inc) was administered to obtain a detailed and comprehensive assessment of verbal learning and memory changes (Delis et al., 2000). The National Institutes of Health Toolbox Cognition Battery (Gershon et al., 2010) assessed attention and inhibitory control, episodic memory, working memory, cognitive flexibility, and processing speed changes and has been validated for use in older adults (Weintraub et al., 2013; Zelazo et al., 2014). Previous and current physical activity habits were assessed using free recall and the Postmenopausal Estrogen/Progestins Intervention (PEPI) Study physical activity questionnaire (Greendale et al., 1996). Self-reported health status change was assessed via the Veterans RAND 12-item Health Survey, a shortened version of the Short Form Health Survey, SF-36, that has been validated for use in military Veterans (Jones et al., 2001; Kazis et al., 1998, 2006). Finally, the Midlife in the United States Survey was used to assess self-reported positive and negative affect (Mroczek & Kolarz, 1998), sense of control (Lachman & Weaver, 1998), and social well-being changes (Keyes, 1998).
Discussion
The Golf Intervention for Veterans Exercise (GIVE) Study was a Phase I longitudinal intervention study that aimed 1) to examine the feasibility, safety, and efficacy of a novel golf-training program on the overall health and well-being of older military Veterans, and 2) to quantify the biomechanical and physical demands of a comprehensive golf intervention. This manuscript provides details about the design of the program and a brief overview of the functional, physical, cognitive, and psychosocial assessments of the participants before and after the intervention.
The United States (U.S.) Department of Veterans Affairs (VA), Greater Los Angeles Healthcare System serves a geographical region with approximately 1.4 million Veterans (United States Department of Veterans Affairs, 2017). According to the VA 2017 census, 50.5% of the Veterans living in California were over the age of 65 years (National Center for Veterans Analysis and Statistics, 2017); therefore, it is approximated that the VA, Greater Los Angeles Healthcare System has the potential to serve 707,000 older military Veterans. Given the poorer health and physical inactivity of older military Veterans (Hoerster et al., 2012; Littman et al., 2009), activity interventions targeting cognitive, physical, and psychosocial health are warranted.
Older adults are motivated to participate in physical activity programs by individual, social, and environmental factors. Individual factors include a motivation to improve overall health, physical function, mental health, and general well-being. Social motivations include encouragement and support from peers. Environmentally, older adults are motivated to participate in a physical activity program if there is the availability of organized exercise programs, particularly if they are specialized for older adults, or to a specific population group (Burton et al., 2017; Cohen-Mansfield et al., 2003).
While golf is a popular recreational activity that can be played across the lifespan, it has been frequently overlooked as a therapeutic physical activity intervention to improve health in older adults. The development of comprehensive golf training programs designed for older adults, and more specifically older military Veterans could address many of the aforementioned motivations for exercise. In the Greater Los Angeles area, golf is both accessible and affordable for older military Veterans. While not an exhaustive list, there are approximately 22 public golf courses located within 5-15 miles of the three primary VA care facilities, with an additional two golf courses being located on VA campuses. The public courses consist of 9- and 18-hole Par 3, Executive, and Regulation golf courses that have practice facilities, including driving ranges and putting greens, and social areas including clubhouses and coffee shops. Auxiliary services include club rentals (~$1/club for a total of $5 for beginner golfers) and golf lessons. Green fees for older adults range from $5-$20 and are dependent upon the number of holes played, course length, and time of play. Implementation of comprehensive golf training programs, similar to those described in this report, would address environmental and individual motivators for exercise by providing a safe and inclusive environment for older military Veterans that prepares them for golf play.
Golf is an accessible activity that contains multiple components that address the physical, cognitive, and psychosocial needs of older military Veterans; however, there is limited information about the utility of a comprehensive golf training program. While a recent randomized control trial demonstrated improved logical memory following completion of a “cognitively focused” 24-week golf program in healthy, older adults, it is uncertain if this program could be feasibly implemented because of its long duration, high staffing requirements, and undescribed home-based practice each day (Shimada et al., 2018). This report allows the golf community, both researchers and instructors, to understand the structure and design of the comprehensive golf training intervention. This information is necessary for the appropriate and comprehensive interpretation of the functional, physical, cognitive, and psychosocial health outcomes utilized.
Acknowledgements
The authors thank the military Veterans that graciously volunteered their time to the GIVE Study, James Dennerline for leading the golf training, and Erin Blanchard for her help with recruitment and development of the complimentary exercises.